How Alcohol Affects the Heart
How does alcohol affect the heart? Does alcohol increase heart rate? It is well established that alcohol can damage every part of your body, including the heart. At The Dunes East Hampton, we have written about how alcohol affects the various organs as a resource for those that are worried about how their drinking is affecting their health now and in the future. For those that are abusing alcohol in large amounts, binge drinking, daily drinking, or drinking for extended periods of time, heart-related symptoms are going to start to show eventually. These symptoms can lead to issues such as alcoholic cardiomyopathy.
When the symptoms of alcohol damage to the heart begin to show, it can be very scary and worrisome for the individual and his or her family. For this reason, we feel it is important to give an overview of how alcohol affects the heart and provide a cumulative resource for those that are worried and fearful about their drinking and heart health.
Note: This article is for informational purposes only and should not be taken as a replacement for seeking treatment and diagnosis from licensed medical practitioners. Consult your doctor regarding alcohol intake and any medical conditions immediately.
When Long-Term Alcohol Abuse Starts to Affect The Heart
Long-term alcohol abuse and binge drinking takes a hard toll on the heart, in several ways:
Increased Heart Rate When Drinking
Alcohol works as a vasodilator, which means that it dilates the blood cells, increases the blood flow within the vessels, and in turn can increase your heart rate. While this effect is only temporary, and often returns to normal within a few hours, any artificial changes to your body’s balance can affect the overall function and balance of the body’s systems – in this case, the cardiovascular system, heart palpitations alcohol connection.
While some studies have shown that, in moderation, alcohol and its vasodilation effects may promote heart health, it is easy to see how this process over and over again, day after day can cause damage and throw off the natural balance the body has created. Often, people have to start a holistic treatment to get their bodies back to this natural balance.
Increased Heart Rate After Drinking: Hangovers and Mild Withdrawal
Alcohol can affect your body’s balance when it is in your bloodstream, but it also affects the way your body works and balances itself when leaving the bloodstream. Your body knows the damage that alcohol can do. To protect itself, the body tries to filter out all of the alcohol from your blood rapidly.
Around 90 percent of the alcohol is processed by the liver, and it processes the alcohol as quickly as it can. This is part of the reason that diseases of the liver are prevalent in heavy drinkers.
However, this quick processing of the alcohol out of the bloodstream means that the body has to once again adjust the balance of its systems again. Many studies point to this second rebalance as the explanation for hangovers: Your weary body is struggling to rebalance while it is dehydrated, tired and suffering minor alcohol damage.
Alcohol and Tachycardia (Persistent Increased Heart Rate)
Tachycardia is a common type of arrhythmia (heart rhythm disorder) where your heart rate remains elevated, even while at rest. People who drink daily or for extended amounts of time will be well aware of this feeling, where your heart feels like it is racing, even though you may just be sitting and doing nothing strenuous that would cause your heart to beat faster.
Tachycardia can be caused by many stimuli – not just alcohol – but alcohol and the fluctuations it causes in heartbeat and dilation of blood vessels can certainly worsen an existing susceptibility to tachycardia and abnormal heartbeat.
Types of tachycardia and heart arrhythmia:
- Atrial Fibrillation (AF)
- Supraventricular Tachycardia (SVT)
- Atrial Flutter
- Ventricular Tachycardia (VT)
- Ventricular Fibrillation
Heart arrhythmia is actually quite common, can occur with or without the abuse of alcohol, and is not always life-threatening or a serious concern. However, the appearance of an arrhythmia tied to alcohol abuse is definitely a warning sign that the alcohol use may be a bigger problem than you realize.
Alcohol and Heart Murmurs
Heart murmurs can be thought of as a “whooshing” between heartbeats. While not often felt by the individual, doctors can usually hear these murmurs while listening to your heartbeat with a stethoscope. Often referred to as a “leaky valve” in layman’s terms, a murmur is often a symptom of an issue with your heart valves.
Just like arrhythmia can be present with or without the use of alcohol, so can murmurs; and just like with arrhythmia, heart murmurs are not always a serious.
Heart murmurs that are not expected to be serious symptoms of other diseases, not considered life-threatening, and not expected to impact one’s quality of life are commonly called “innocent murmurs.” However, alcohol CAN damage heart muscles and valves, and valve damage – or worsening of existing valve damage – can be caused by heavy alcohol abuse.
‘Holiday Heart’ and Alcohol-Related Arrhythmia
While some studies have fallen short of saying definitively that alcohol abuse directly causes heart arrhythmia, other studies have shown that those with alcohol use disorders are more likely to be diagnosed with, or have a higher risk of developing, a heart arrhythmia. We do know for certain that there is a link between alcohol and arrhythmia, and that alcohol, caffeine and other substances tend to have an effect on the severity of the symptoms of abnormal heartbeat.
“Holiday heart” is a term that doctors coined in response to the annual increase in doctor visits they receive during and after Christmas and the holiday season. This season coincides with an increase in celebrating and often a heavy increase in alcohol use. Patients often complain of chest pains, tightness in the chest or possible heart fluttering. Some even say that they are worried that they might be having a heart attack.
In these holiday heart cases, the main suspect is usually alcohol. In the majority of such cases, the individual usually has a minor (and often undiagnosed) heart arrhythmia, tachycardia, high blood pressure or another heart-related issue that has been exacerbated by an increase in alcohol use.
Alcoholic Cardiomyopathy, Heart Failure, and Serious Heart Damage from Alcohol
Up until this point, we have covered some of the less-serious affects that alcohol causes on the heart, or heart issues that are common, but can be worsened by alcohol abuse.
 And by “less serious” we should clarify that we mean that though these issues are commonly associated with alcohol abuse, they are not always fatal, are often treatable, can in many cases be reversed, don’t often impact the quality of life, or the progression can be slowed with abstinence from alcohol. Some effects of alcohol on the heart, however, are much more serious.
And by “less serious” we should clarify that we mean that though these issues are commonly associated with alcohol abuse, they are not always fatal, are often treatable, can in many cases be reversed, don’t often impact the quality of life, or the progression can be slowed with abstinence from alcohol. Some effects of alcohol on the heart, however, are much more serious.
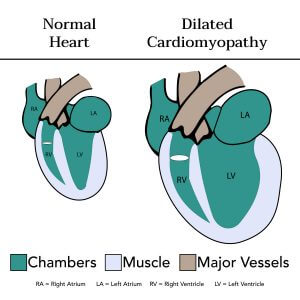
Cardiomyopathy is the umbrella name given to diseases of the heart muscle. Sometimes the heart disease can be tied back to a worsening arrhythmia, alcohol heart palpitations, and tachycardia. Sometimes the heart muscles have been damaged and the heart walls are thinning to the point where the danger of heart failure looms. Other times, such as with alcoholic cardiomyopathy, the root of the cardiomyopathy is damage to the heart muscle that has left the heart enlarged or covered in scar tissue (common with heavy alcohol abuse).
When heart disease is tied directly to alcohol abuse, it is referred to as alcoholic cardiomyopathy. This is the more serious stage of damage to the heart, where the heart itself is heading towards the symptoms of heart failure. In many cases, the proper cessation from alcohol and change of lifestyle can slow the progression of alcoholic cardiomyopathy symptoms, though in severe cases, the heart failure is inevitable and irreversible. In these cases, a heart transplant may be considered.
Alcohol and Heart Palpitations or Other Symptoms
Along with alcoholic cardiomyopathy, there are a number of other heart problems you can experience. If you have had a history of heavy drinking and found this article because you wanted to learn more about the heart symptoms affecting you, this article has either calmed your nerves a bit or has made you more worried. The good news is that much of the damage alcohol can do to your heart can be reversed or controlled, and alcoholic cardiomyopathy (which cannot be reversed) is much rarer than other forms of alcohol-induced heart issues. In fact only upwards of 30% of all cardiomyopathy cases are alcoholic cardiomyopathy.
While it may seem like you are the only one worried that your drinking his causing you heart-related worries, palpitations, elevated pulse and tachycardia, nearly everyone who has abused alcohol for long periods of time will end up in the same position.
So now that your body is sending warning signs that alcohol has been causing damage, what do you do next? The first thing to do is go and talk to your doctor about your concerns. Once you have that first honest conversation with a medical professional (and tell them the real amount you have been drinking), you will be very relieved to know that you are not the only one that comes in complaining of heart palpitations, pains or other cardiovascular issues that may be tied to drinking too much.
Once you have this conversation with your doctor he will most likely take your vitals, order blood tests, and possibly give you an ECG (Electrocardiogram). At this point, regardless of whether the issues are serious or less serious, it will be time to look at your options for cutting back on your drinking or to completely taper alcohol out of your routine.
Alcohol Withdrawal Heart Dangers and Safe Medical Detox from Alcohol
Just as your heart is affected – and your blood pressure and heart rate can increase – after a night of drinking, your heart can be affected by the decision to STOP after years of drinking. Alcohol is the most dangerous substance to quit “cold turkey,” and the withdrawals from alcohol can be deadly. The risk of seizures, heart failure, severe heart arrhythmias and other deadly symptoms are extremely high when stopping or even tapering off of alcohol. This is why it is essential to detox from alcohol under the supervision of a medical professional under medically assisted alcohol detox. Simply put – there is no other way to safely stop drinking alcohol than a medically assisted alcohol detox.
Heart Palpitations After Detox and Lingering Heart Symptoms in Alcohol Recovery
If an underlying condition such as heart palpitations, liver damage, or any other ancillary disease that was worsened by alcohol abuse is the reason for detox and recovery from alcohol, ensuring that you are under medical care during detox and throughout the first 6-12 months of your recovery is also essential.
While undergoing medically assisted detox and stopping the use of alcohol can stop the progression of or possibly reverse the symptoms of your heart issues, this will likely take time. While your body will attempt to quickly rebalance itself after stopping (causing the most extreme and deadly symptoms of withdrawal) within the first weeks of recovery, the body can take even longer to full re-balance itself.
Depending on how long you have been drinking and how much, a full recovery could take months or years. The underlying conditions – such as heart palpitations and arrhythmias – will also take time to slowly get back to normal. The important thing to remember is that your body is reversing years of damage caused by alcohol, and just as you are re-learning how to function in a healthy manner, so is your body. Proper nutrition in recovery can help this process along, and it is important to keep your doctor informed of any changes in your health.
Problems like heart palpitations and alcoholic cardiomyopathy aren’t to be taken lightly. Keep your doctor up to date on any and all symptoms you experience, even if you think they’re small. It’s better to mention something minor than to overlook something that may be a major problem.
When Your Body Tells You To Quit Drinking
When your body begins to show signs of the damage alcohol has done, and your body seems to be telling you that something is wrong – whether it be with your heart, liver, lungs, or other organs – it can be terrifying, and your instinct is to think the worst. But, the body is both resilient and intelligent, and symptoms from alcohol abuse are often the body moving from “telling” you to cut out the alcohol to “screaming at you” that you need to make a change. Before alcoholic cardiomyopathy becomes a permanent part of your life, be sure that you listen to your body’s pleas, speak honestly to your doctor, detox safely under medical supervision, begin to reverse the damage, and keep focused on recovery.
If you have questions about alcohol addiction treatment, be sure to check out our FAQs or give us a call today to learn more about us and our luxury rehab center.